|
Case Report
Shoulder and arm pain: A “red herring” chief complaint in a smoker diagnosed with Pancoast-Tobías syndrome
1 MD, Department of Community Health and Psychiatry, Faculty of Medical Sciences, The University of the West Indies, Mona Campus, Kingston 7, Jamaica
2 MD, Department of Anesthesia and Intensive Care, Bustamante Hospital for Children, Kingston, Jamaica
3 MD, National Blood Transfusion Services, Kingston, Jamaica
4 MD, Independent Researcher, Fort Worth, TX 76104, USA
5 MD, Department of Emergency Medicine, The University Hospital of the West Indies, Kingston 7, Jamaica
Address correspondence to:
Chadane Thompson
MD, Department of Community Health and Psychiatry, Faculty of Medical Sciences, The University of the West Indies, Mona Campus, Kingston 7,
Jamaica
Message to Corresponding Author
Article ID: 100127Z10CT2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Thompson C, Daley R, Fullerton S, Lambert-Johnson S, Johnson DK. Shoulder and arm pain: A “red herring” chief complaint in a smoker diagnosed with Pancoast-Tobías syndrome. J Case Rep Images Oncology 2024;10(1):1–6.ABSTRACT
Introduction: A Pancoast tumor is a rare apical lung cancer that can lead to a constellation of signs and symptoms known as Pancoast-Tobías syndrome, which involves ipsilateral shoulder and arm pain, Horner’s syndrome, and atrophy of the intrinsic hand muscles. As a Pancoast tumor progresses, it first invades the brachial plexus and causes unrelenting shoulder and arm pain in the C8-T2 nerve distributions. However, when evaluating this presenting symptom, it is often considered benign, especially in aging patients. Consequently, Pancoast-Tobías syndrome is easily misdiagnosed or delayed in diagnosis, resulting in poor prognosis, particularly for patients with advanced disease.
Case Report: We present the case of an elderly Afro-Caribbean woman with a 24-pack-year smoking history who presented with unrelenting pain to the right shoulder and arm for two months. During that time, she visited multiple family physicians. Onset of pain coincided with a wasp sting that was complicated by a large local reaction. Despite clinical resolution of the inflammatory reaction, the pain persisted even with multi-modal oral analgesics. Detailed physical examination later revealed ipsilateral atrophy of the intrinsic hand muscles and focal chest findings concerning for an underlying consolidative lung process. This prompted diagnostic chest imaging, which identified a right-sided Pancoast tumor aggressively invading adjacent structures. She soon developed Horner’s syndrome, resulting in clinicoradiologic confirmation of Pancoast-Tobías syndrome.
Conclusion: It is important to consider Pancoast-Tobías syndrome as an important differential of unrelenting shoulder and arm pain, even in the absence of pulmonary symptoms, in patients with risk factors for lung cancer, such as chronic smokers.
Keywords: Arm pain, Lung cancer, Palliative care, Pancoast-Tobías syndrome, Pancoast tumor, Shoulder pain, Smoker
Introduction
A Pancoast tumor is a rare apical lung cancer, accounting for approximately 3–5% of all lung cancers [1],[2],[3]. Pancoast-Tobías syndrome is a rare clinical condition that results from an underlying Pancoast tumor invading adjacent structures such as the brachial plexus, superior sympathetic chain, and stellate ganglion, thereby producing ipsilateral shoulder and arm pain, Horner’s syndrome (the classic triad of ptosis, miosis, and facial hemianhidrosis), and atrophy of the intrinsic hand muscles [1],[2],[3],[4],[5]. Most Pancoast tumors are classified as either squamous cell carcinomas (45–50%), adenocarcinomas (36–38%), or undifferentiated large-cell carcinomas (11–13%) [6]. However, the rates of adenocarcinomas have been increasing as of recently.
Since Pancoast tumors first invade the brachial plexus, unrelenting shoulder and arm pain is the most common initial symptom in up to 96% of cases [1],[2],[3],[4]. Moreover, pulmonary symptoms are usually absent due to the peripheral location of these tumors [4]. This peculiar initial presentation of Pancoast-Tobías syndrome can be misleading and causes misdiagnosis or diagnostic delay [1],[3],[5]. As a result of this problem and the burden of the disease itself, Pancoast tumors bring a poor prognosis with a 30% survival rate at five years [1],[3].
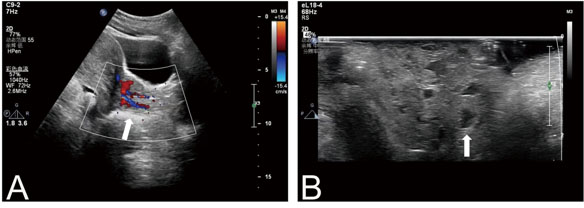
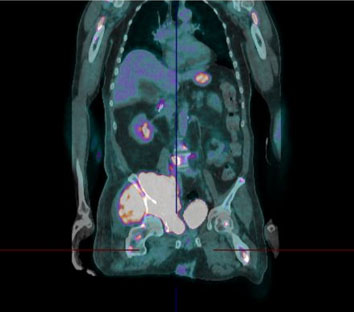
Ninety percent of Pancoast tumors can be diagnosed with clinicoradiologic methods alone [5]. Initially, a chest X-ray can be done in patients with a suspicious history or physical examination. The chest X-ray typically demonstrates findings consistent with an apical lung mass, but it can be negative in 1.7% of cases [7]. More detailed scans, such as a computed tomography (CT) scan or magnetic resonance imaging (MRI), can better detail the extent of a Pancoast tumor and provide local staging [1],[3][5]. Magnetic resonance imaging has the added benefit of being more sensitive and specific in delineating the degree of neurovascular and bony tissue involvement and is most useful imaging modality for surgical planning of resectable tumors. Definitive diagnosis is usually by CT-guided transthoracic needle biopsy to determine the histopathology of the Pancoast tumor and this method has greater than 90% yield [1]. Evaluation for hepatic, bone, and brain metastasis is a key component of staging studies, usually established with positron emission tomography-computed tomography (PET-CT).
Suffice to say, management of Pancoast-Tobías syndrome requires personalized treatment goals and a multidisciplinary approach with medical oncologists, thoracic surgeons, radiation oncologists, pulmonologists, and palliative care professionals. The gold standard treatment includes trimodality treatment, which involves a combination of induction chemoradiation (with platinum-based chemotherapy regimens and radiotherapy) followed by radical resection in 4–6 weeks post-radiation [1],[2],[4]. Alongside this, adequate pain management is paramount, as this is the earliest and one of the most debilitating symptoms. Treatment carries a two-year survival rate of 55–70% [8]. However, since Pancoast tumors are commonly diagnosed after significant invasion has occurred, only less than half of patients have resectable disease at presentation [5]. Moreover, locoregional relapse post-treatment is common. In patients with non-resectable disease, there is still benefit from full dose chemotherapy and interval assessment for resectability versus consolidation chemotherapy [1].
Herein, we describe a delayed diagnosis of Pancoast-Tobías syndrome that was initially missed in an elderly Afro-Caribbean woman with multiple presentations for a chief complaint of unrelenting shoulder and arm pain.
Case Report
A 67-year-old Afro-Caribbean woman presented to the community clinic with a complaint of two months of severe right shoulder and arm pain. She reported that the pain radiated in an ulnar nerve dermatomal distribution and started around the time that she suffered a wasp sting to the proximomedial right arm. At that instance, she had developed a large localized inflammatory reaction at the site of injury. The signs of inflammation eventually resolved except for the pain, which was described as an “unbearable, cramping sensation” that worsened at night and disrupted sleep. She initially attempted to self-medicate with herbal remedies and acetaminophen 1 g four times/day, but this provided no relief. During the two-month course leading up to this presentation, she had visited multiple different family physicians. She was prescribed diclofenac sodium 50 mg three times/day, pregabalin 75 mg twice/day, and eventually acetaminophen-codeine phosphate 1000 mg-60 mg three times/day. There was limited response to all these oral analgesics, even when combined. Her condition was initially thought to be a mixture of age-related shoulder osteoarthritis and sequelae of the wasp sting.
Additionally, she was a retired construction worker and actively smoked cigarettes with a 24-pack-year history. She also consumed approximately three drinks of alcohol daily for over 48 years. There was no hoarseness, hemoptysis, dyspnea, chronic cough, headaches, seizures, fever, weight loss, night sweats, or fatigue reported. There was no family or personal history of malignancy. All prior requests for age-appropriate cancer screening investigations were not fulfilled.
Physical examination revealed a woman of slender habitus in moderate painful distress. There was no cyanosis, icterus, or lymphadenopathy. Her vital signs were within normal limits except a respiratory rate of 22 breaths per minute and a blood pressure of 140/80 mmHg. There was no right upper limb edema or gross deformity to the right shoulder. However, there was tenderness to the right clavicle and right anterior chest wall, with pain-limited range of motion at the shoulder. The right anterosuperior chest wall was dull to percussion with decreased breath sounds to the right apex. Her neurologic examination revealed motor weakness throughout the right upper extremity and impaired fine motor skills in the hands with atrophy of the hypothenar eminence. There were no other abnormalities on physical examination.
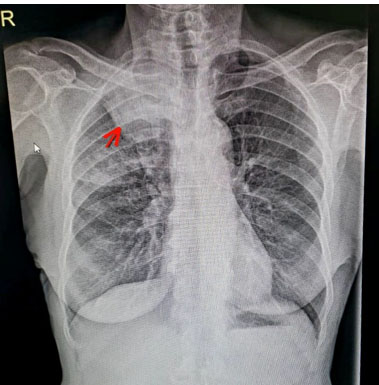
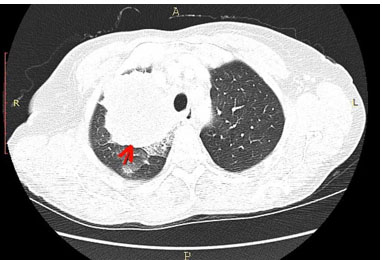
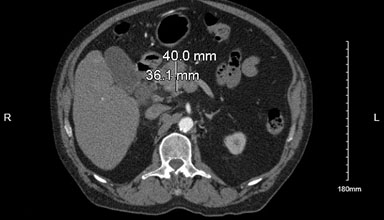
Her baseline blood investigations were normal. X-ray of the right shoulder showed early degenerative changes to the coracoclavicular joint and a right apical lung opacity. Further evaluation with upright posteroanterior and lateral views of the chest on plain X-ray showed a wedge-shaped opacified area of ground glass changes in the right upper lung zone, just proximal to the horizontal fissure (Figure 1). The impression gained from the X-rays prompted an urgent chest computed tomography (CT) scan to better evaluate the right apical lung focus. The chest was imaged using CT in the arterial phase. A 7.8 cm (L) × 8.0 cm (W) 7.1 cm (AP) loculated, heterogenous mass within the apical segment of the right upper lobe was found (Figure 2). There was an associated non-displaced pathological fracture of the neck of the first rib with irregularity of its inferior cortex. The mass was predominantly hypodense, with thick irregular peripheral enhancement and invasion into adjacent pleura. There were associated crazy paving changes involving the right upper and middle lobes in keeping with tumor spread. The left lung was unremarkable. No effusions were present. The mass also abutted the right lateral wall of the esophagus. The fat plane between the structures was intact, with patency of the esophagus maintained. Large right lower paratracheal and right hilar nodes were seen. The right subclavian vein and artery were preserved in outline with no evidence of stenosis or filling defect. These findings were consistent with a Pancoast tumor.
The patient was referred for multi-disciplinary specialist management in a tertiary care hospital. She declined any conventional medical treatments and sought alternative therapies alongside opioid analgesia. A lung biopsy and staging scans were also not obtained. Within a month, she developed gait instability and right-sided Horner’s syndrome. Given her characteristic findings of right-sided shoulder and arm pain, atrophy of the intrinsic hand muscles, and Horner’s syndrome alongside radiographic evidence of an ipsilateral Pancoast tumor, the diagnosis of Pancoast-Tobías syndrome was made. She eventually died four months later due to disease progression.
Discussion
In clinical practice, shoulder pain is one of the most common complaints voiced, especially among aging patients, with an estimated prevalence of 4–26% and the significant majority of cases are of benign musculoskeletal, rheumatologic, or neurologic origin [9]. However, it is important to remain aware that shoulder pain may be the initial presentation of a serious underlying condition such as a Pancoast tumor.
In our patient, there was likely an element of premature closure by previous physicians in concluding that her shoulder pain was partly due to osteoarthritis, by virtue of her age. Though our patient was elderly and had evidence of early degenerative changes to the right coracoclavicular joint on plain radiographs, ipsilateral shoulder and arm pain was in fact the initial presenting symptom of the underlying Pancoast tumor. This serious condition was also disguised by the fact that she had suffered a wasp sting with a large local reaction to the affected extremity. This was also thought to be contributing to her pain since a large local reaction can leave residual symptoms. However, the unremitting nature of her symptoms requiring escalation to opioids despite clinical resolution of the inflammatory reaction should have prompted an alternative explanation to challenge the issue of anchoring bias. Another confounder was that our patient did not endorse respiratory symptoms such as cough, hemoptysis, or dyspnea and this is typical of Pancoast-Tobías syndrome [4]. Her chest findings were also subtle and could easily be missed, especially if the focus of the physical exam were the musculoskeletal system. Additionally, the finding of Horner’s syndrome, a key clinical sign that often accompanies 15–50% of cases [2], was not present until later in the disease course. The patient’s behavior of “doctor hopping and shopping” also contributed to her diagnostic delay, as no single physician was involved with ongoing assessment of her response to prescribed interventions. Similar reports of underlying Pancoast tumors in older patients with a significant smoking history have been described and these patients were often misdiagnosed or diagnosed late, which reinforce the need for maintaining a high index of suspicion in this demographic of patients when they present with shoulder and arm pain [7],[10],[11],[12].
Though Pancoast-Tobías syndrome is most commonly caused by primary or secondary apical lung malignancies, it is also important to consider other differentials of apical lung masses [13], including (i) infectious diseases (tuberculosis, Staphylococcus, Pseudomonas, thoracic actinomycosis, aspergillosis, echinococcosis, allescheriasis, cryptococcosis, and hydatid cyst), and (ii) miscellaneous medical conditions (neurofibromatosis, cervical rib syndrome, vascular aneurysms, and amyloid nodules). Because of this wide variation of etiologies of Pancoast-Tobías syndrome, it is necessary to obtain a biopsy to prove the underlying histologic diagnosis. However, following radiographic confirmation of the likely Pancoast tumor in our patient, a biopsy was not obtained to confirm the histopathological subtype of the lung mass since the patient declined this procedure.
Furthermore, our patient opted to choose alternative medicine over conventional therapies, despite thorough counseling. In medicine, the opinions on the utility of alternative medicine are diverse, particularly in serious illnesses such as cancer. Ultimately, in cancer treatment, there is an established standard of care based on more standardized and evidence-based principles, but consideration of the cultural context also plays a role in establishing personalized treatment goals. A patient’s choice to integrate alternative medicine should be guided by informed dialogues with the care team with special emphasis on all existing scientific data, its potential risks and benefits, and its limitations in halting disease progression compared with standard of care.
It is also important to understand that early incorporation of palliative care in patients with serious illnesses is paramount for improved quality of life and optimal patient outcomes. Pancoast tumors are most commonly of the non-small cell variety [1],[2],[3],[4]. It has been shown that for people with newly diagnosed metastatic non-small cell lung cancer, early integration of palliative care alongside standard oncologic care improves quality of life, lessens depression, lessens aggressive end of life care, and increases survival by an average of 2.7 months compared with those who received standard oncologic care alone [14]. However, despite our patient being managed in a tertiary hospital, dedicated in-house palliative care services were still not readily available. Notably, in many low- and middle-income countries such as those in the Caribbean, there is inadequate incorporation of palliative care into existing health systems and shortage of trained palliative care professionals, leading to limited availability of essential palliative care services, particularly within the framework of cancer care [15]. Therefore, a focus on prioritizing palliative care training and education of healthcare workers, lobbying for support from policy makers and palliative care leaders, and establishing strategic partnerships to improve access to, affordability of, and equitable distribution of culturally sensitive palliative care services is needed in the Caribbean [15]. With these interventions, there could be substantial strides in improving the quality of life of patients in the region with serious or life-limiting illnesses.
The earlier that Pancoast tumors are detected and treated, the better the prognosis but emphasis must also be placed on disease prevention [1],[3],[8]. Since these tumors are usually bronchogenic, patients typically have a smoking history, as did our patient. Her chronic alcohol use, advanced age, and potential carcinogenic occupational exposures as a retired construction worker were also risk factors for development of lung cancer. Especially in at-risk populations, healthcare professionals should reinforce preventive strategies such as smoking cessation, prevention of smoking initiation, and use of annual low-dose chest CT scan in those who fulfil screening criteria. The latest guideline set forth by the United States Preventive Services Task Force (USPSTF) recommends annual lung cancer screening with low-dose CT in adults aged 50–80 years with a 20-pack-year smoking history, who currently smoke or have quit in the past 15 years (Grade B recommendation) [16]. Unfortunately, our patient did not fulfil routine screening investigations that could have led to earlier diagnosis. To date, lung cancer stands as the leading cause of cancer-related mortality globally, and promotion of routine screening allows for timely and life-saving interventions.
Conclusion
Ipsilateral shoulder and arm pain is the most frequent initial symptom seen in Pancoast-Tobías syndrome. This common presentation of an uncommon disease entity typically results in misdiagnosis and diagnostic delay. This case emphasizes the importance of considering chest imaging to investigate for Pancoast-Tobías syndrome as a differential of unrelenting shoulder and arm pain, particularly in chronic smokers who are at increased risk for lung cancer. Additionally, careful assessment for the co-existence of Horner’s syndrome and atrophy of intrinsic hand muscles is key in eliciting the diagnosis. Early diagnosis, staging, and prompt initiation of trimodality treatment (chemotherapy, radiotherapy, and surgery) alongside palliative care approaches can improve overall survival and quality of life. Moreover, the importance of primary and secondary prevention of lung cancer must be underscored in routine clinical practice.
REFERENCES
1.
Villgran VD, Chakraborty RK, Cherian SV. Pancoast Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
[Pubmed]

2.
Marulli G, Battistella L, Mammana M, Calabrese F, Rea F. Superior sulcus tumors (Pancoast tumors). Ann Transl Med 2016;4(12):239. [CrossRef]
[Pubmed]

3.
Gundepalli SG, Tadi P. Lung Pancoast Tumor. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
[Pubmed]

4.
5.
Panagopoulos N, Leivaditis V, Koletsis E, et al. Pancoast tumors: Characteristics and preoperative assessment. J Thorac Dis 2014;6(Suppl 1):S108–15. [CrossRef]
[Pubmed]

6.
Foroulis CN, Zarogoulidis P, Darwiche K, et al. Superior sulcus (Pancoast) tumors: Current evidence on diagnosis and radical treatment. J Thorac Dis 2013;5(Suppl 4):S342–58. [CrossRef]
[Pubmed]

7.
Al Shammari M, Hassan A, Al Jawad M, et al. Pancoast tumor: The overlooked etiology of shoulder pain in smokers. Am J Case Rep 2020;21:e926643.
[Pubmed]

8.
Latimer KM, Mott TF. Lung cancer: Diagnosis, treatment principles, and screening. Am Fam Physician 2015;91(4):250–6.
[Pubmed]

9.
Murphy RJ, Carr AJ. Shoulder pain. BMJ Clin Evid 2010;2010:1107.
[Pubmed]

10.
Sayeed A, Alshamrani FMM, Amrayn AY, Alharbi A. Shoulder pain in smokers could be a life changer. BMJ Case Rep 2017;2017:bcr2017220969. [CrossRef]
[Pubmed]

11.
Ronan L, D’Souza S. Pancoast’s tumour presenting as shoulder pain in an orthopaedic clinic. BMJ Case Rep 2013;2013:bcr2012008131. [CrossRef]
[Pubmed]

12.
Shanmugathas N, Rajwani KM, Dev S. Pancoast tumour presenting as shoulder pain with Horner’s syndrome. BMJ Case Rep 2019;12(1):e227873. [CrossRef]
[Pubmed]

13.
Arcasoy SM, Jett JR. Superior pulmonary sulcus tumors and Pancoast’s syndrome. N Engl J Med 1997;337(19):1370–6. [CrossRef]
[Pubmed]

14.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363(8):733–42. [CrossRef]
[Pubmed]

15.
Stoltenberg M, Spence D, Daubman BR, et al. The central role of provider training in implementing resource-stratified guidelines for palliative care in low-income and middle-income countries: Lessons from the Jamaica Cancer Care and Research Institute in the Caribbean and Universidad Católica in Latin America. Cancer 2020;126 Suppl 10:2448–57. [CrossRef]
[Pubmed]

16.
US Preventive Services Task Force; Krist AH, Davidson KW, et al. Screening for Lung Cancer: US preventive services task force recommendation statement. JAMA 2021;325(10):962–70. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Chadane Thompson - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rebecca Daley - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sidni Fullerton - Conception of the work, Design of the work, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shana-Kay Lambert-Johnson - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Donahue Krisstoff Johnson - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from a legally authorized representative for anonymized patient information to be published in this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Chadane Thompson et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.