|
Case Report
Esthetic and functional treatment with a lithium disilicate crown: A case report
1 Professor, Department of Restorative Dentistry, University of Santo Amaro, São Paulo, SP, Brazil
2 MSc Student, Department of Biological Sciences, Bauru School of Dentistry, University of São Paulo, Bauru, SP, Brazil
3 PhD, Department of Restorative Dentistry, Piracicaba Dental School, University of Campinas, Campinas, SP, Brazil
4 MSc, Department of Dental Clinic, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
5 Adjunct Professor, Department of Dental Clinic, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
6 PhD, Department of Dental Clinic, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
7 Associate Professor, Department of Dental Clinic, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
8 DDS, Gama Filho University, Rio de Janeiro, RJ, Brazil
9 Professor, Department of Dental Clinic, School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Address correspondence to:
João Victor Frazão Câmara
Alameda Doutor Octávio Pinheiro Brisolla, 6-65, CEP 17012-059, Bauru, São Paulo,
Brazil
Message to Corresponding Author
Article ID: 101187Z01JP2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Pierote JJA, Câmara JVF, Barbosa IF, Vianna RFC, Tinoco JMM, Fried H, Santos AEC, Castro AN, Pereira GDS. Esthetic and functional treatment with a lithium disilicate crown: A case report. Int J Case Rep Images 2020;11:101187Z01JP2020.ABSTRACT
Introduction: Lithium disilicate-based ceramics are extensively used in restorative dentistry, considering these materials combines adequate mechanical and optical properties, which, associated with dentin bonding by resin luting cement, makes them suitable for load-bearing posterior regions. This case report aims to describe the clinical and laboratory steps of a ceramic crown restoration.
Case Report: A 30-year-old female patient had the second right maxillary premolar restored with lithium disilicate. The tooth was conditioned with phosphoric acid 37, followed by washing with water and drying with air jet. After this stage, the adhesive was applied to the surface and blasted with air. The prosthetic part was prepared with 10% hydrofluoric acid on the internal surface, washed with water, application of silane and adhesive. For definitive cementation, resinous cementing agent was used on the internal surface, the excess was removed and photopolymerization was performed.
Conclusion: This case report represents a successful esthetic treatment and shows resistant ceramic restorations that can be placed over minimally invasive tooth preparations.
Keywords: Aesthetic rehabilitation, Aesthetic treatment, Lithium disilicate porcelain
Introduction
Dentistry has evolved over the past decades to meet increasingly demanding esthetic and functional needs from patients [1],[2]. New restorative materials and techniques for both direct and indirect restorations have been developed and improved [3],[4]. However, studies on the biomechanical behavior of these materials are still necessary to confirm whether they fulfill the requirements of masticatory function [5].
The ideal restorative material should fulfill functional and esthetic requirements while offering long-term stability [6]. Although direct resin composite restorations present acceptable color matching [7], adequate mechanical properties [8], easy repair [9], and longevity in the clinical service [10], there are still concerns regarding the potential effects of inherent polymerization shrinkage stresses related to these materials, which could lead to marginal staining, loss of marginal seal, microleakage, secondary caries, enamel cracks, postoperative sensitivity, cusp fracture, and restoration failure [11].
Therefore, indirect all-ceramic restorations are better suited in the case of wide cavities with extensive tissue destruction, especially in endodontically treated teeth. Glass-ceramics present improved mechanical properties compared to resin composites, less shrinkage stress (of the resin luting cement), and optimal esthetic features with long-lasting shade match [12].
Thus, this case report aims to describe the clinical steps regarding the performance of the ceramic crown technique.
Case Report
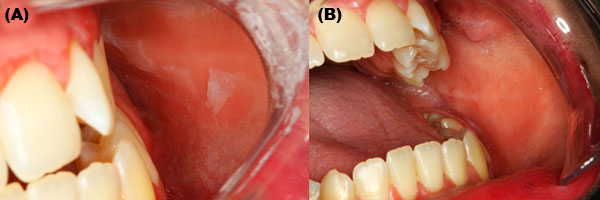
A 30-year-old female patient attended the Dental Clinic complaining of tooth appearance. The clinical examination showed a coronary fracture in tooth 25, reaching the lingual and distal walls, as well as the presence of caries on the distal aspect, without painful symptoms (Figure 1A). The digital radiographic evaluation showed that endodontic treatment was successfully performed without the need for retreatment (Figure 1B).
Thus, considering the patient’s aesthetic requirement, the treatment plan consisted of producing a lithium disilicate ceramic crown due to the lack of integrity of the surrounding walls, aided by a fiberglass post to provide greater stability and mechanical resistance. After discussing the case, the patient signed the Free and Informed Consent Form.
Initially, the oral environment was adapted, in which supragingival and subgingival scrapings were performed to eliminate tartar and guide oral hygiene to ensure the quality of life and proper maintenance of teeth.
Then, posterior upper alveolar anesthesia was performed and the dental surfaces were cleaned. For root canal preparation, the filling material was removed at least for the same crown measure and preparation was performed with a wide #3 Gates drill. Then, 37% phosphoric acid etching was performed for 15 seconds (Ultradent Products, SP, Brazil), followed by washing and drying with a paper cone (Figure 2A, Figure 2B, Figure 2C). The adhesive was applied (Single Bond, 3M ESPE, Brazil) and paper cones were used for excess removal (Figure 2D and Figure 2E). Then light curing (Valo Cordless, Ultradent Products, SP, Brazil) was performed for 40 seconds (Figure 2F). The intraradicular post was cleaned with phosphoric acid for 10 seconds, followed by washing, drying, and silane application (Figure 2G). After 3 minutes, the adhesive was applied in the canal, dried by air spray, and light-cured for 15 seconds. The cement (RelyX U100 3M ESPE, Brazil) was inserted in the canal with a lentulo spiral, positioning the post with the help of clinical tweezers (Figure 2H). The excess cement was removed and light-curing was performed for 40 seconds.
The full crown preparation was characterized by a cervical end in a rounded shoulder with the aid of a 4138 diamond tip drill (KG Sorensen, Brazil) (Figure 2I and Figure 2J). After completing the preparation, the impression was made with the help of two retraction threads from Ultrapak with a caliber compatible with the gingival groove. The threads used were 00 and 0, and the thinner one (thread 00) was maintained during molding (Figure 2K and Figure 2L). The impression material used was addition silicone (Silicona Elite Zhermack). Before cementing, the crown was tested to check the color and adaptation to the dental structure (Figure 3A), and then prophylaxis was performed with pumice and water. In the prosthetic part, 10% hydrofluoric acid (FGM Produtos Odontológicos) was applied for 1 minute, followed by washing and drying with air spray on the adhesive (Single Bond, 3M ESPE) (Figure 3B). Silane was maintained for 60 seconds and then air-dried (Figure 3C). The self-adhesive cement RelyX U100 3M ESPE was inserted inside the ceramic crown, the excess cement was removed (Figure 3D and Figure 3E), and, after 3 minutes, photoactivation was performed for 40 seconds on each surface. After cementation, occlusal adjustment (Figure 3E and Figure 3F) and polishing with abrasive tips for ceramics and digital radiography were performed (Figure 4A and Figure 4B).
Discussion
The longevity of dental restorations is affected by several factors such as material properties, patient behavior, technique acuity, and operator skills during the clinical steps [13].
Over the years, the formulation of resin-based composites has evolved. As a result, their mechanical and optical properties improved. However, polymerization shrinkage remains one of the main problems related to the use of this material on direct techniques, especially in the case of great losses of tooth structure [14]. To prevent the side effects of polymerization shrinkage, which may result in cracks, gaps, and marginal leakage in the remaining dental tissue, direct resin composites may not be indicated to restore extensively compromised teeth. In such cases, indirect restorations are recommended and may be produced with indirect resin composite or dental ceramics [15].
Indirect systems allow the extraoral production of restorations, which not only strengthens the mechanical and physical properties of the restorative material but also prevents residual monomer development. Furthermore, indirect restorations do not require all the inconveniences inherent to direct restoration procedures, e.g., operatory field isolation, protection of adjacent teeth with metal strips, and recovery of proximal contacts. This ensures a reliable marginal adaptation, simplifies the restorative process, and saves time to both operator and patient [16].
The digital radiographs performed in this case report have the main advantages of reducing working time and reducing the radiation dose. The technology uses radiation-sensitive circuit boards, which send the captured image directly to the computer. In this way, there is no need for film development or a digitizer [17].
Ceramics are characterized by physical and mechanical properties such as microhardness and thermal and electrical insulation, as well as optical properties, therefore representing a high translucent material. They also present surface smoothness and degradation resistance, which enable color stability and restoration integrity over time. These features also contribute to the compatibility with periodontal tissues. The most used ceramics in dentistry are oxides, particularly silicon dioxide, aluminum oxide, and zirconium dioxide, which are suited for several types of indirect restorations: inlays, onlays, full-coverage crowns, laminates, fixed partial dentures, and implant abutments [18].
Adding dispersed lithium disilicate crystals to the glass matrix of feldspathic ceramics increased the mechanical properties without compromising optical properties [19]. Lithium disilicate-based materials are remarkable among dental glass-ceramics and extensively used for crowns due to their high flexural strength and, due to its translucency, it can be used to manufacture monolithic restorations, completely anatomical and with integral contour. The high strength makes it ideal for making inlays, onlays, thin veneers, anterior partial crowns, posterior crowns, bridges in three anterior units, bridges and implant superstructures up to the second premolar. However, it requires special care with the crown and bridge design so that it has a minimum material thickness of 0.8 mm and a connection area of 16 mm² [20]. Nonetheless, lithium disilicate ceramics can mimic hard dental tissues and present sufficient mechanical properties to support their use in partial preparations of posterior teeth [20].
Conclusion
Considering the clinical case presented, it may be concluded that lithium disilicate-based ceramics are indicated for indirect crowns because this type of dental ceramic presents adequate mechanical and optical properties that will lead to clinical success, restoring health, esthetics, and masticatory function to patients.
REFERENCES
1.
Yao J, Tang H, Gao X L, McGrath C, Mattheos N. Patients’ expectations to dental implant: A systematic review of the literature. Health Qual Life Outcomes 2014;12:153. [CrossRef]
[Pubmed]

2.
Cosyn J, Thoma DS, Hämmerle CHF, De Bruyn H. Esthetic assessments in implant dentistry: Objective and subjective criteria for clinicians and patients. Periodontology 2017;73(1):193–202. [CrossRef]
[Pubmed]

3.
Vaderhobli RM. Advances in dental materials. Dent Clin North Am 2011;55(3):619–25. [CrossRef]
[Pubmed]

4.
Li RWK, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: State of the art. J Prosthodont Res 2014;58(4):208–16. [CrossRef]
[Pubmed]

5.
Zhang YR, Du W, Zhou XD, Yu HY. Review of research on the mechanical properties of the human tooth. Int J Oral Sci 2014;6(2):61–9. [CrossRef]
[Pubmed]

6.
Ilie N, Hickel R. Resin composite restorative materials. Aust Dent J 2011;56 Suppl 1:59–66. [CrossRef]
[Pubmed]

7.
Mourouzis P, Koulaouzidou EA, Palaghias G, Helvatjoglu-Antoniades M. Color match of resin composites to intact tooth structure. J Appl Biomater Funct Mater 2015;13(3):e259–65. [CrossRef]
[Pubmed]

8.
Ferracane JL. Resin composite—State of the art. Dent Mater 2011;27(1):29–38. [CrossRef]
[Pubmed]

9.
Ruse ND, Sadoun MJ. Resin-composite blocks for dental CAD/CAM applications. J Dent Res 2014;93(12):1232–4. [CrossRef]
[Pubmed]

10.
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJM. Longevity of posterior composite restorations: Not only a matter of materials. Dent Mater 2012;28(1):87–101. [CrossRef]
[Pubmed]

11.
Fronza BM, Rueggeberg FA, Braga RR, et al. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent Mater 2015;31(12):1542–51. [CrossRef]
[Pubmed]

12.
Politano G, Fabianelli A, Papacchini F, Cerutti A. The use of bonded partial ceramic restorations to recover heavily compromised teeth. Int J Esthet Dent 2016;11(3):314–36.
[Pubmed]

13.
Batalha-Silva S, de Andrada MA, Maia HP, Magne P. Fatigue resistance and crack propensity of large MOD composite resin restorations: direct versus CAD/CAM inlays. Dent Mater. 2013;29(3):324–31. [CrossRef]
[Pubmed]

14.
Nikolaenko SA, Lohbauer U, Roggendorf M, Petschelt A, Dasch W, Frankenberger R. Influence of c-factor and layering technique on microtensile bond strength to dentin. Dent Mater 2004;20(6):579–85. [CrossRef]
[Pubmed]

15.
Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res 1984;63(12):1396–9. [CrossRef]
[Pubmed]

16.
Li RWK, Chow TW, Matinlinna JP. Ceramic dental biomaterials and CAD/CAM technology: State of the art. J Prosthodont Res 2014;58(4):208–16. [CrossRef]
[Pubmed]

17.
Khorasani MMY, Ebrahimnejad H. Comparison of the accuracy of conventional and digital radiography in root canal working length determination: An invitro study. J Dent Res Dent Clin Dent Prospects 2017;11(3):161–5. [CrossRef]
[Pubmed]

18.
Tapie L, Lebon N, Mawussi B, Fron-Chabouis H, Duret F, Attal J. Understanding dental CAD/CAM for restorations – accuracy from a mechanical engineering viewpoint. [Article in English, French]. Int J Comput Dent 2015;18(4):343–67.
[Pubmed]

19.
Gorman CM, Horgan K, Dollard RP, Stanton KT. Effects of repeated processing on the strength and microstructure of a heat-pressed dental ceramic. J Prosthet Dent 2014;112(6):1370–6. [CrossRef]
[Pubmed]

20.
Anadioti E, Aquilino SA, Gratton DG, et al. Internal fit of pressed and computer-aided design/computer-aided manufacturing ceramic crowns made from digital and conventional impressions. J Prosthet Dent 2015;113(4):304–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Josué Junior Araujo Pierote - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
João Victor Frazão Câmara - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Isabel Ferreira Barbos - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Renato Feres de Carvalho Vianna - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Justine Monteiro Monnerat Tinoco - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hana Fried - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Amara Eulalia Chagas Santos - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adriano Nóbrega de Castro - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Gisele Damiana da Silveira Pereira - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Josué Junior Araujo Pierote et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.