|
Case Report
A rare case report of extra medullary plasmacytoma involving the posterior mediastinum coexistent with multiple myeloma
1 PGY2 Resident, MD, Department of Internal Medicine, The Brooklyn Hospital, Center Clinical Affiliate of Mount Sinai Hospital, 121 Dekalb Avenue, Brooklyn, NY, USA
2 Fellow in Hematology and Oncology, Department of Hematology and Oncology, The Brooklyn Hospital Center clinical affiliate of Mount Sinai Hospital, 121 Dekalb Avenue, Brooklyn, NY, USA
Address correspondence to:
Lohitha Dhulipalla
PGY2 Resident, MD, Department of Internal Medicine, The Brooklyn Hospital, Center Clinical Affiliate of Mount Sinai Hospital, 121 Dekalb Avenue, Brooklyn, NY 11201,
USA
Message to Corresponding Author
Article ID: 100088Z10LD2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Dhulipalla L, Karki M, Huq A, Rana A. A rare case report of extra medullary plasmacytoma involving the posterior mediastinum coexistent with multiple myeloma. J Case Rep Images Oncology 2021;7:100088Z10LD2021.ABSTRACT
Introduction: Plasma cell neoplasms are characterized by the clonal proliferation of plasma cells. They include monoclonal gammopathy of undetermined significance, multiple myeloma, and solitary osseous or non-osseous plasmacytoma. Multiple myeloma is characterized by the proliferation of plasma cells in the bone marrow and can result in extensive skeletal destruction, whereas plasmacytoma is characterized by the proliferation of plasma cells restricted to one area of the body.
Case Report: A 65-year-old female presented for workup of incidental mass noted on computed tomography (CT) of the chest. She was noted to have posterior mediastinal plasmacytoma with elevated IgA and free lambda light chains on serum electrophoresis. She subsequently underwent the bone marrow biopsy which revealed multiple myeloma. The patient was diagnosed with IgA lambda multiple myeloma with a posterior mediastinal plasmacytoma with multiple bony lesions. She underwent radiotherapy with interval resolution of posterior mediastinal mass and currently on chemotherapy for multiple myeloma.
Conclusion: Once plasmacytoma is diagnosed, a further workup for multiple myeloma is needed as treatment is entirely different for both types of plasma cell neoplasms.
Keywords: Extramedullary plasmacytoma, Extramedullary plasmacytoma coexistent with multiple myeloma, Medullary plasmacytoma, Multiple myeloma, Plasmacytoma
Introduction
Plasmacytoma is a rare type of neoplasm of plasma cells. It can manifest as primary plasmacytoma or secondary associated with multiple myeloma. Primary plasmacytoma is of two types: medullary plasmacytoma (involving the bone marrow) and extramedullary plasmacytoma (involving the soft tissues). The incidence of extramedullary plasmacytoma is 3% of all plasma cell neoplasms [1],[2],[3]. About 5% of case of extramedullary plasmacytomas have coexistent multiple myeloma [2]. Here we report a rare case of extramedullary plasmacytoma involving the mediastinum coexistent with multiple myeloma.
Case Report
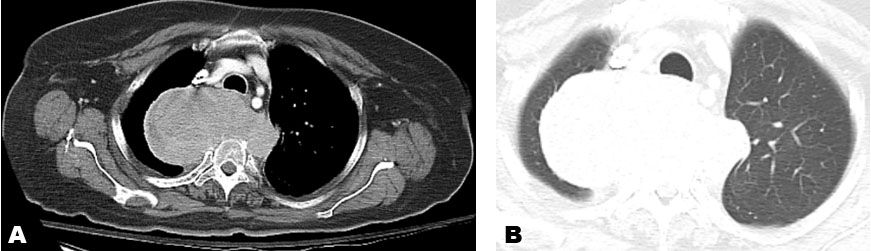
A 65-year-old woman presented to the hospital for further workup of an incidental mass found on computed tomography (CT) chest. The patient had also suffered a fall a week before the presentation. The patient was admitted and further workup was done. Computed tomography chest axial (Figure 1A and Figure 1B) revealed 6.7 by 11.2 × 6.6 cm sagittal by transverse by AP posterior mediastinal mass having a mass effect upon the trachea which was deviated anteriorly. Destructive changes within the T3 and T4 vertebra with soft tissue extension into the spinal canal at this level with marked compression of the spinal cord were noted. Sub-carinal, prominent right paratracheal, and pre-vascular lymph nodes were noted. The patient underwent an interventional radiology (IR)-guided biopsy of the posterior mediastinal mass. Pathology report of large soft tissue posterior mediastinal mass revealed plasmacytoma. Serum protein electrophoresis showed elevated IgA immunoglobulins and free lambda chains. The skeletal survey showed multiple diffusely scattered lytic disease. The patient subsequently underwent bone marrow biopsy which revealed features suggestive of plasma cell dyscrasia (with the involvement of bone marrow by atypical plasma cells 60–70% of total cellularity).
The whole-body bone scan revealed a pathological fracture of the left proximal femur associated with malignant invasion into the surrounding soft tissue, large ovoid photon deficient area on the left side of T3, T4, and T5 vertebrae, and adjacent left posterior rib cage; consistent with complete bony destruction by the adjacent posterior mediastinal mass lesion was noted. Multiple compression fractures found at T2, L3, and L5 vertebrae (Figure 2). The patient was diagnosed with IgA lambda multiple myeloma with a posterior mediastinal plasmacytoma with multiple bony lesions.
She underwent radiation therapy and was on Cyclophosphamide, Bortezomib, and Dexamethasone chemotherapy from 01/2020 to 08/2020. Repeat CT chest (Figure 3A and Figure 3B) after radiotherapy revealed interval resolution of previously seen associated paravertebral soft tissue mass; currently on maintenance Velcade. She is currently tolerating the treatment well and is being closely followed up.
Discussion
Primary plasmacytoma is of two types. The medullary plasmacytoma arises from the bone marrow and the extramedullary plasmacytoma which usually arises in the soft tissues of the head and neck and upper respiratory tract and rarely gastrointestinal tract, liver, spleen, pancreas, breast, and skin [2]. Extramedullary plasmacytoma involving posterior mediastinum is very rare. Only a few people with extramedullary plasmacytoma have coexistent multiple myeloma. Here we report a case of extramedullary plasmacytoma involving the mediastinum coexistent with multiple myeloma.
The mainstay of treatment of primary plasmacytoma is surgery and has a good prognosis. Extramedullary plasmacytoma is radiosensitive and is treated with radiotherapy [2]. The mainstay of treatment of multiple myeloma is chemotherapy or autologous hematopoietic stem cell transplantation. Multiple myeloma usually has a poor prognosis. Here our patient underwent radiotherapy with interval resolution of paravertebral soft tissue mass and currently on maintenance therapy for multiple myeloma and is responding well [2].
Conclusion
Extramedullary plasmacytoma involving the mediastinum is rare. Once plasmacytoma is diagnosed, further workup for multiple myeloma is needed as treatment is entirely different for both types of plasma cell neoplasms. Plasmacytomas are treated with surgery, radiotherapy, or both. Treatment refractory cases are treated with chemotherapy. Multiple myeloma is treated with chemotherapy. In our patient, further workup of incidental mass leads to the diagnosis of multiple myeloma.
LIST OF ABBREVIATIONS
AP anteroposterior
T3 - Thoracic vertebra T3
T4 - Thoracic vertebra T4
T5 - Thoracic vertebra T5
L3 - Lumbar vertebra
L5 - Lumbar vertebra
IgA - Immunoglobulin A
REFERENCES
1.
Masood A, Hudhud KH, Hegazi A, Syed G. Mediastinal plasmacytoma with multiple myeloma presenting as a diagnostic dilemma. Cases J 2008;1(1):116. [CrossRef]
[Pubmed]

2.
Lee SY, Kim JH, Shin JS, et al. A case of extramedullary plasmacytoma arising from the posterior mediastinum. Korean J Intern Med 2005,20(2);173–6. [CrossRef]
[Pubmed]

3.
Miyazaki T, Kohno S, Sakamoto A, et al. A rare case of extramedullary plasmacytoma in the mediastinum. Intern Med 1992;31(12):1363–5.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Lohitha Dhulipalla - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Monika Karki - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ammar Huq - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Anshuma Rana - Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Lohitha Dhulipalla et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.