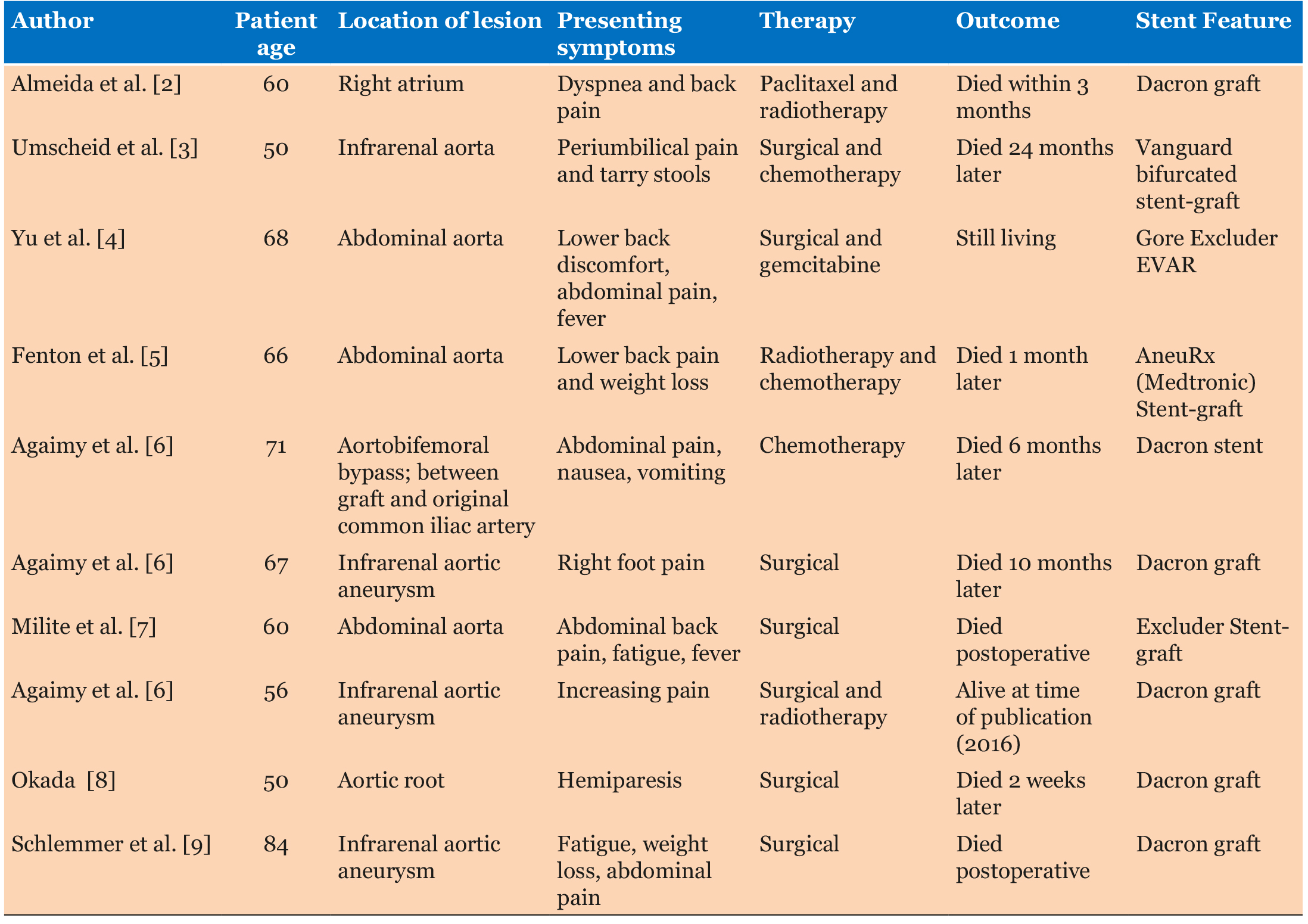
|
Case Report
Primary angiosarcoma of the aorta in association with an endurant stent graft
1 Medical Student, College of Osteopathic Medicine, Midwestern University, Glendale, AZ, USA
2 Hospitalist, Internal Medicine, Banner Health, Banner Estrella Medical Center, Phoenix, AZ, USA
3 Hematology/Oncology, Medical Oncology and Hematology, Ironwood Cancer and Research Centers, Avondale, AZ, USA
Address correspondence to:
Ashley Almajan
19555 N 59th Ave, Glendale, AZ 85308,
USA
Message to Corresponding Author
Article ID: 100075Z10AA2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Almajan A, Parveen P, Saraceni C. Primary angiosarcoma of the aorta in association with an endurant stent graft. J Case Rep Images Oncology 2021;7:100075Z10AA2021.ABSTRACT
Introduction: Angiosarcomas are extremely rare tumors, especially those arising in the aorta.
Case Report: We uniquely present a case where primary aortic angiosarcoma was found in a 68-year-old woman in association with an Endurant stent graft.
Conclusion: Only a handful of cases have shown an association between the development of primary angiosarcoma and other endovascular grafts, such as a Dacron stent graft. However, this may be the first case to report an association with an endurant stent graft.
Keywords: Angiosarcoma, Aorta, Endurant, Graft, Stent
Introduction
Primary aortic sarcomas present very rarely with only about 145 cases reported to date. Among these, the subset of primary aortic angiosarcoma is only around 34 reported cases [1]. We uniquely present a case where primary aortic angiosarcoma was found in association with an endurant stent graft. Only a handful of cases have shown an association between the development of primary angiosarcoma and other endovascular grafts, such as a Dacron stent graft [2] (Table 1). However, this may be the first case to report an association with an endurant stent graft.
Little is known about how to correlate clinical presentation, diagnosis, and treatment options specific to this cancer. Often masquerading as aortoiliac occlusive disease, acute thromboembolism or false saccular aneurysm, pathologic examination is crucial to confirming this diagnosis [1]. Angiosarcomas commonly arise in the inner lining of blood vessels of the head and neck area, breast, bone, liver, spleen, or the lymphatic endothelium. Therefore, angiosarcomas of the aorta are not always suspected due to low incidence rate.
Case Report
A 69-year-old woman initially presented with severe chronic back pain and difficulty with ambulation. She had previously undergone an endovascular abdominal aortic aneurysm repair and three years later was found to have a persistent endoleak of the endoluminal stent. An angiogram with embolization of multiple lumbar branches of the inferior mesenteric artery was performed. A few weeks later, a computed tomography (CT) angiogram of the abdomen and pelvis revealed a persistent small endoleak within the anterior inferior aspect of the aneurysm and a small periaortic hematoma. An esophagogastroduodenoscopy and colonoscopy were performed due to severe anemia and were unremarkable.
She was noted to be markedly anemic with a hemoglobin of 6.6 g/dL. Thrombocytosis was present with a platelet count of 476,000 and a persistent leukocytosis with white blood cells in the 20,000 range. Peripheral blood flow cytometry was unremarkable. She was discharged as there was no extravasation on multiple imaging studies to suggest aneurysm rupture.
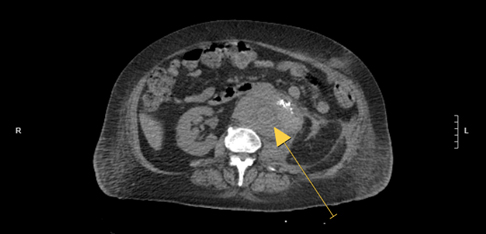
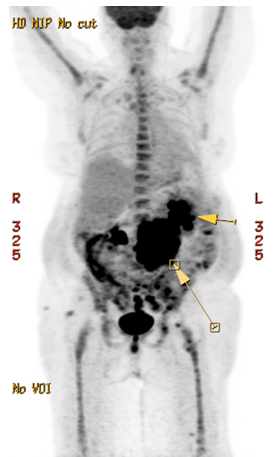
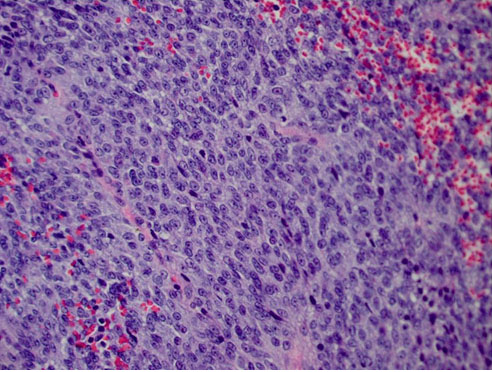
A few months later she was electively admitted for a periaortic soft tissue mass, initially felt to be aortic hematoma (Figure 1). She underwent an open repair of a juxtarenal abdominal aortic aneurysm with a Dacron stent and aortobiiliac bypass with explantation of previously placed Endurant endovascular stent graft and splenectomy. Pathology from the splenectomy did not show evidence of malignancy. Pathology from the thrombus and plaque from the stent graft was positive for CD31, erythroblast transformation specific related gene (ERG), Wilms tumor (WT), and vimentin consistent with poorly differentiated angiosarcoma. Positron emission tomography (PET) scan showed widely metastatic disease (Figure 2) involving the length of the aorta and the left iliac fossa lymph nodes (Figure 3). The soft tissues of the right buttock, distal left thigh, pelvic bones, and left femur showed metastases. Small left pleural effusion and bibasilar opacities were seen. Bone marrow biopsy was negative for involvement of angiosarcoma. Brain magnetic resonance imaging (MRI) did not show intracranial metastases. She was started on Pazopanib 400 mg daily but had progressive clinical disease within 6 weeks. She was readmitted and subsequently started on weekly paclitaxel. She shortly opted for hospice care and passed three months after initial diagnosis.
Discussion
Angiosarcomas represent about 2% of all soft tissue sarcomas [10] and very rarely do they originate in the aorta. When they do originate in the aorta, they frequently present in the descending thoracic aorta (35%), followed by abdominal aorta (27%), thoracoabdominal aorta (27%) and less frequently in the ascending aorta or arch (11%) [11]. Other sarcomas found specific to the aorta include leiomyosarcoma, myofibrosarcoma, fibromyxosarcoma, hemangioendothelioma, and rhabdomyosarcomas [12]. Aortic angiosarcomas can be further subdivided depending on where they arise (polypoidal, intraluminal, intimal, medial, or adventitial). The polypoidal and intraluminal types often cause luminal obstruction or thrombus formation [11] while adventitial sarcomas typically do not cause obstruction by themselves [13]. Intimal sarcomas, being the most common, are characterized by spindle cells displaying atypia, pleomorphism, and necrosis often form intraluminal polyps that lead to aortic obstruction or formation of peripheral emboli [11]. Sarcomas originating from the media will often present as mural tumors with extravascular growth; the smooth muscle cells of the medial layer also being the origin to leiomyosarcomas [14].
Risk factors
There are several predisposing factors for the development of angiosarcoma. Radiation therapy, chronic lymphedema, chemicals, and certain familial syndromes all increase likelihood of occurrence. Radiation-induced angiosarcoma of the breast has been especially documented. A study by Senen et al. reported an incidence of 0.9 per 1000 breast cancer cases occurring with a median of seven years after radiation therapy [15]. In addition, chronic lymphedema (Stewart-Treves syndrome) has been linked secondary to Milroy’s disease, filariasis, or postsurgery/radiotherapy [16]. Different chemicals including vinyl chloride, thorium dioxide, arsenic, and anabolic steroids can increase risk [3]. In fact, 25% of all primary hepatic angiosarcoma cases were associated with these chemicals [16]. Lastly, familial syndromes including Neurofibromatosis (NF-1), mutated BRCA1 or BRCA2, Maffucci syndrome, and Klippel-Trenaunay syndrome predispose to development of angiosarcoma [10].
Association with other grafts or foreign material
Dacron vascular grafts have been associated with other primary sarcomas. Examples include epithelioid angiosarcoma at the site of an aortobifemoral bypass, malignant fibrous histiosarcoma of the aorta after repair of a thoracic aortic dissection, hemangiosarcoma following endovascular aortic aneurysm repair, and fibrosarcoma [2],[3]. Dacron mitral valve prosthesis has been associated with several cases of malignant cardiac tumors including a case of malignant fibrous histiocytoma, a lymphoma, and angiosarcoma [2]. One case found an association between primary cardiac angiosarcoma and an autologous saphenous vein graft [17]. Primary angiosarcomas have also been associated with ruptured silicone breast implants [18] orthopedic implants, arteriovenous fistulas, and dialysis shunts [2].
Foreign body properties including type of material, shape, size, porosity, smoothness, hardness, and electrostatic load influence carcinogenic potential. Tumorigenesis is likely due to the presence of synthetic polyester material in the body [13]. A pore diameter of less than 0.4 um is associated with increased risk of tumor development [10].
Diagnosis
Computer tomography (CT), magnetic resonance imaging (MRI), and transesophageal echocardiography (TEE) have been used to diagnose angiosarcoma. Computed tomography imaging may show protrusive vegetations or discrete soft-tissue mass with lobules often shaped like a “cauliflower” [19]. Often, these bulky lesions will cause intraluminal narrowing that can be mistaken for a tumor, thrombus or atheroma. Symptoms of visceral occlusive disease will warrant a CT or CTA scan on initial work-up. If there are signs of brachiocephalic insufficiency or aortic coarctation symptoms, then a TEE should be performed [20]. Magnetic resonance imaging has been shown to be superior to help distinguish an intimal sarcoma from atherosclerotic disease [9]. Common markers including CD31, CD34, factor VIII, and Fii-1 are used in immunohistochemical studies to help make this diagnosis [9].
The presenting symptoms can be nonspecific including abdominal pain, back pain, lower extremity claudication, and secondary hypertension [14]. Other symptoms may include weight loss, bleeding, fatigue, depending on the sites of the disease.
Treatment
At initial presentation, the majority of patients (>50%) will have metastatic disease predominantly to the lungs and subsequently the liver followed by, chest wall, skin, brain, bone, and intestines [10]. The median survival of patients with angiosarcoma of the aorta is 14 months from time of diagnosis (ranging from 1–75 months) [10]. A combination of surgical resection, chemotherapy, and radiation offers the longest survival time. Surgical resection should be performed with a margin of at least 2 cm of unaffected tissue surrounding the tumor for best results. Treatment for primary angiosarcoma of the aorta is tailored individually depending on age, comorbidities, performance status, and age of the disease. One patient was treated with surgical resection and radiation but died 16 months later [10]. Another was treated with surgical resection, mitomycin, doxorubicin, cisplatin and did not recur at a 16 year follow-up [16]. Another was treated with mitomycin C, doxorubicin, and cisplatin but died four months later [10]. According to Fatima et al., patients receiving any combination of surgical resection, radiation, or chemotherapy lived at least five months from the time of diagnosis while one patient who only underwent surgical resection lived two months [20]. However, one patient did not receive any form of therapy but lived 20 months from diagnosis [15]. The use of paclitaxel in patients with metastatic angiosarcomas according to Schlemmer et al. has shown a response rate of 75% (6/8) in scalp angiosarcomas and 58% (14/24) in other sites of primary angiosarcoma [9].
Conclusion
Angiosarcomas of the aorta are rare entities. An association with medical devices and endovascular stents has been suggested. Presenting signs and symptoms can be non-specific, often leading to a misdiagnosis. Angiosarcoma can mimic aortoiliac occlusive disease, thromboembolism, or false saccular aneurysm. Due to the rarity of angiosarcoma, the optimal treatment is not yet defined but multimodality approaches combining surgery, chemotherapy, and radiation are used. The prognosis, despite these therapies is dismal.
REFERENCES
1.
Ramjee V, Ellozy S. Aortic angiosarcoma masquerading as a thoracic aortic aneurysm. J Vasc Surg 2009;50(6):1477–80. [CrossRef]
[Pubmed]

2.
Almeida NJ, Hoang P, Biddle P, Arouni A, Esterbrooks D. Primary cardiac angiosarcoma: In a patient with a Dacron aortic prosthesis. Tex Heart Inst J 2011;38(1):61–5.
[Pubmed]

3.
Umscheid TW, Rouhani G, Morlang T, et al. Hemangiosarcoma after endovascular aortic aneurysm repair. J Endovasc Ther 2007;14(1):101–5. [CrossRef]
[Pubmed]

4.
Yu PC, Aplin B, Reed AB. Angiosarcoma of the abdominal aorta after endovascular aneurysm repair. J Vasc Surg Cases Innov Tech 2019;5(4):506–8. [CrossRef]
[Pubmed]

5.
Fenton J, Veenstra M, Bove P. Angiosarcoma involving native abdominal aortic aneurysm sac after endograft repair. Ann Vasc Surg 2014;28(2):e1–4. [CrossRef]
[Pubmed]

6.
Agaimy A, Ben-Izhak O, Lorey T, Scharpf M, Rubin BP. Angiosarcoma arising in association with vascular Dacron grafts and orthopedic joint prostheses: Clinicopathologic, immunohistochemical, and molecular study. Ann Diagn Pathol 2016;21:21–8. [CrossRef]
[Pubmed]

7.
Milite D, Pilon F, Ferrari A, Danieli D, Desole A. Aortic epithelioid angiosarcoma after endovascular aneurysm repair. Ann Vasc Surg 2016;35:207.e17–21. [CrossRef]
[Pubmed]

8.
Okada F. Beyond foreign-body-induced carcinogenesis: Impact of reactive oxygen species derived from inflammatory cells in tumorigenic conversion and tumor progression. Int J Cancer 2007;121(11):2364–72. [CrossRef]
[Pubmed]

9.
Schlemer M, Reichardt P, Verweij J, et al. Paclitaxel in patients with advanced angiosarcomas of soft tissue: A retrospective study of the EORTC soft tissue and bone sarcoma group. Eur J Cancer 2008;44(16):2433–6. [CrossRef]
[Pubmed]

10.
Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol 2010;11(10):983–91. [CrossRef]
[Pubmed]

11.
Lin SI, Su MI, Tsai CT. Primary intimal sarcoma of thoracic aorta presenting as hypertensive crisis. Acta Cardiol Sin 2015;31(6):560–3. [CrossRef]
[Pubmed]

12.
Neri E, Miracco C, Luzi P, Carone E, Tripodi A, Sassi C. Intimal-type primary sarcoma of the thoracic aorta presenting as a saccular false aneurysm: Report of a case with evidence of rhabdomyosarcomatous differentiation. J Thorac Cardiovasc Surg 2005;118(2):371–2. [CrossRef]
[Pubmed]

13.
Salm R. Primary fibrosarcoma of aorta. Cancer 1972;29(1):73–83. [CrossRef]
[Pubmed]

14.
15.
Seinen JM, Styring E, Verstappen V, et al. Radiation-associated angiosarcoma after breast cancer: High recurrence rate and poor survival despite surgical treatment with R0 resection. Ann Surg Oncol 2012;19(8):2700–6. [CrossRef]
[Pubmed]

16.
Zhu YP, Chen YM, Matro E, et al. Primary hepatic angiosarcoma: A report of two cases and literature review. World J Gastroenterol 2015;21(19):6088–96. [CrossRef]
[Pubmed]

17.
Hartvigson PE, Velamoor GR, Loggers ET, Kim E. Cardiac angiosarcoma from a saphenous vein coronary artery bypass graft. Cureus 2019;11(8):e5503. [CrossRef]
[Pubmed]

18.
Smoll NR, Farhadieh RD, Ferguson R, Findlay MW, Hunter-Smith DJ. High-grade angiosarcoma associated with ruptured breast implants. Plast Reconstr Surg Glob Open 2013;1(1):e11–3. [CrossRef]
[Pubmed]

19.
Gaballah AH, Jensen CT, Palmquist S, et al. Angiosarcoma: Clinical and imaging features from head to toe. Br J Radiol 2017;90(1075):20170039. [CrossRef]
[Pubmed]

20.
Fatima J, Duncan AA, Maleszewski JJ, et al. Primary angiosarcoma of the aorta, great vessels, and the heart. J Vasc Surg 2013;57(3):756–64. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Ashley Almajan - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Parveen Parveen - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Christine Saraceni - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Ashley Almajan et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.