|
Case Report
Recurrence of pleomorphic adenoma of the maxilla 14 months after resection: A case report
1 The State Key Laboratory Breeding Base of Basic Science of Stomatology (Hubei-MOST) & Key Laboratory of Oral Biomedicine Ministry of Education, School & Hospital of Stomatology, Wuhan University, #237 Luoyu Road, Wuhan 430079, China
Address correspondence to:
Ke Liu
The State Key Laboratory Breeding Base of Basic Science of Stomatology (Hubei-MOST) & Key Laboratory of Oral Biomedicine Ministry of Education, School & Hospital of Stomatology, Wuhan University, #237 Luoyu Road, Wuhan 430079,
China
Message to Corresponding Author
Article ID: 100073Z10YZ2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Zhang Y, Wang L, Liu K. Recurrence of pleomorphic adenoma of the maxilla 14 months after resection: A case report. J Case Rep Images Oncology 2020;6:100073Z10YZ2020.ABSTRACT
Introduction: Salivary gland tumors account for 3% of head and neck tumors, often in the salivary glands, such as the parotid gland and the salivary gland. The most common pathological type is pleomorphic adenoma.
Case Report: The salivary gland tumors, which occurred in the jaws of the jaw, were developed from the glandular tissue in the jaws of the jaw, and the clinical and imaging examinations made the lesion similar to that of the dental source, and it was easy to be confused with other diseases in the clinical diagnosis.
Conclusion: This paper reports a rare pleomorphic adenoma of the maxilla.
Keywords: Adenocarcinoma, Intraosseous salivary gland tumor, Malignant mixed tumor, Pleomorphic adenoma, Recurrence, The maxilla
Introduction
Pleomorphic adenoma, also called mixed tumor, is a kind of tumor containing glandular tissue, mucus, and cartilage-like tissue, because the structure of the tissue is diverse, it is called “mixed tumor.” It is the most common salivary gland benign tumor, about 80% in the parotid gland and 20% in the minor salivary glands. Pleomorphic adenoma is mostly seen in the young, generally has no obvious self-conscious symptoms, the growth is slow, and the course of the disease can be up to several years or even decades. Ectopic salivary gland tumors can occur at different sites, including the skin, the neck, the thyroid, the mastoid, the maxilla, the mandible, and the like. Benign salivary gland tumors in the jaws of the jaw are very rare, with only a few cases reported. Since the clinical and imaging performance of this type of tumor is similar to that of the dental source, strict evaluation criteria are used to avoid misdiagnosis.
Case Report
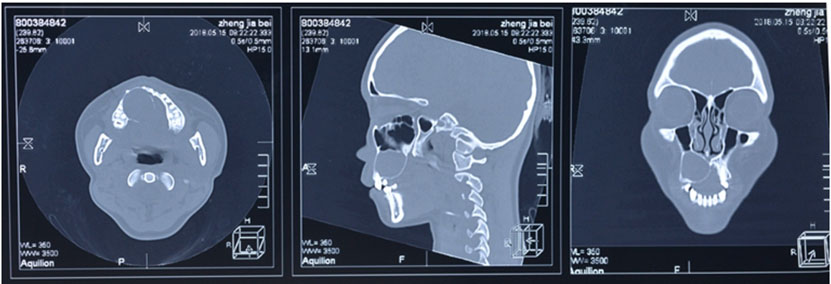
A 17-year-old female presented with the main complaint was “One month after right maxillary hard palate tumor.” One year ago, the patient underwent the “hard palatine mass resection” in the external hospital, and the results showed that pleomorphic adenoma (no capsule). One month ago the patient was aware of right auditory allergy, cone beam computer tomography (CBCT) examination showed that the local bone absence of the right maxillary bone was seen with isodensity (Figure 1). In order to seek further treatment, the patient came to our hospital.
Operation: Complete the inspection before operation and eliminate the contraindication of the operation. In general anesthesia, the conventional disinfection and drape shall be performed. The upper jaw-side bone surface depression is visible in the gingival flap on the side of the 17–25 mm side. The soft tissue lesion is visible in it, and the swelling is completely separated from the bone surface (Figure 2). The gum flap was turned up on the labial side of 15–21, and the root side of 14–11 was concave and connected to the wound on the palatine side, and soft tissue masses could be seen near the middle, so the masses were peeled off, the root of 15–11 area was trimmed and the bone edge of the root was sharp, and then part of the maxillary bone was removed by grinding the head to avoid residual lesion tissue.
Pathological description: The connective tissue of the fiber was arranged in a ring, and the proliferation of the fiber was obviously like a scar-like change. There were a few epithelial stripes and epithelial fissures in it. The epithelial lesions showed local infiltrative growth and no capsule. Regional adenotubular differentiation was found, but there was no obvious heteromorphism in cancer cells.
The patient has been followed up on a monthly basis for 12 months now, without evidence of recurrence so far.
Discussion
The intraosseous salivary gland tumor is rare. The most common is the mucoepidermoid carcinoma, followed by adenoid cystic carcinoma, malignant mixed tumor, pleomorphic adenoma, adenocarcinoma not otherwise specified (NOS), acinar cell carcinoma, and pleomorphic adenoma [1]. Pleomorphic adenomas originated in the middle of the jaw are extremely rare. In one review of 138 cases of central salivary gland tumors, only 5 cases of intraosseous pleomorphic adenomas were found [2]. Although central pleomorphic adenomas are relatively rare, oral professionals should be aware of this possibility and emphasize the need to submit so-called cystic lesions for histopathological analysis. Various theories explain on the origin of intraosseous salivary gland tumors, most of which involve the possible tumor transformation of ectopic salivary gland tissue, which originates from embryonic residues of developed primary or secondary gland [3]. It also has been found that the central type of salivary gland has more than a dental cyst or a tooth barrier. Different intraosseous gland tumors may also originate from soft tissue salivary gland tumors invading the jaw. In order to diagnose intraosseous salivary gland tumors, certain prerequisites must be met [4]. First, there must be no primary or concurrent primary tumor in the large salivary gland or the small salivary gland. Second, there should be evidence of osteolysis but complete cortical bone, and finally a positive histological diagnosis of salivary gland tumors [5],[6]. Although the clinical and radiological features of this case show dental origin, the histopathological evidence is the gold standard for the final diagnosis of pleomorphic adenoma. Metastatic pleomorphic adenoma is defined as local or distant metastasis of histologically benign pleomorphic adenoma. The five-year disease-specific and disease-free survival rates were 58% and 50%, respectively. It is estimated that about 20–40% of microscopic polyangiitis (MPA) patients end up dying from the disease. Pleomorphic adenomas usually have multiple recurrence history, at least twice or more, before the formation of metastases, but some scholars have also reported that there is no recurrence before the formation of metastases [7]. There are different opinions on the origin of the salivary gland tumors of the maxilla.
In this case, first, the head and neck were not found to have pre-existing or co-existing similar tumors; second, the case showed that the exact criteria for not meeting the requirements for complete cortical bone were not continuous on partial axial imaging of the lateral palatal cortex, but may be due to the patient having undergone hard palatal mass resection a year ago, resulting in a discontinuity in the palatal cortex. Postoperative pathological diagnosis was also confirmed as pleomorphic adenoma because these lesions occur in the structure of the tooth supporting bone and are usually closely related to the teeth, clinical and radiologic are similar to odontogenic cysts, thus, they are prone to misdiagnosis in clinical diagnosis.
Conclusion
Although the clinical and radiologic features of this case show odontogenic lesions, histology is proved to be the gold standard for the final diagnosis of atypical pleomorphic adenomas. Surgery is considered to be the first choice for the treatment of intraosseous pleomorphic adenoma.
REFERENCES
1.
Aghaghazvini L, Aghaghazvini S. Intraosseous pleomorphic adenoma of the mandible. Iran J Radiol 2015;12(1):e6921. [CrossRef]
[Pubmed]

2.
Akiba J, Harada H, Kawahara A, Todoroki K, Nagata S, Yano H. A case of metastasizing pleomorphic adenoma in the maxillary bone appearing twenty years after initial resection of pleomorphic adenoma of the hard palate. Pathol Int 2013;63(9):463–8. [CrossRef]
[Pubmed]

3.
Alshagroud R, Kamoh A, Popat SR, Brandwein-Weber M, Aguirre A. Metastasizing pleomorphic adenoma case report and review of the literature. Head Neck Pathol 2017;11(4):487–93. [CrossRef]
[Pubmed]

4.
Buva KB, Deshmukh AA, Deshmukh AA. A case report of rare carcinoma ex pleomorphic adenoma of submandibular gland and its detailed description. J Clin Diagn Res 2017;11(5):ZD15–7. [CrossRef]
[Pubmed]

5.
Ide F, Mishima K, Kikuchi K, Miyazaki Y, Kusama K. Primary intraosseous myoepithelioma of the mandible with ameloblastomalike features. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114(6):e49–53. [CrossRef]
[Pubmed]

6.
Mallika L, Augustine D, Sagar P, Prasad K, Rao RS. Pleomorphic adenoma masquerading as odontogenic lesion in the Maxilla. J Clin Diagn Res 2017;11(8):ZJ01–2. [CrossRef]
[Pubmed]

7.
Ojha J, Bhattacharyya I, Islam MN, Manhart S, Cohen DM. Intraosseous pleomorphic adenoma of the mandible: Report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104(2):e21–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Yu Zhang - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lin Wang - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ke Liu - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Yu Zhang et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.