Case Series
Superior mesenteric artery syndrome in oncology: Report of two cases and review of the literature
1 Clinical Nutrition Department, National Institute of Cancer, Santiago, Chile
2 Clinical Nutrition Department, National Institute of Cancer, Santiago, Chile
3 Clinical Nutrition Department, National Institute of Cancer, Santiago, Chile
4 MD, Radiology Department, National Institute of Cancer, Santiago, Chile
5 Clinical Nutrition Department, National Institute of Cancer, Santiago, Chile
Address correspondence to:
Simona Minzer
MD, Clinical Nutrition Department, National Institute of Cancer, Profesor Zañartu 1010, Independencia, Santiago,
Chile
Access full text article on other devices

Access PDF of article on other devices

Article ID: 100130Z10SM2024
doi: 10.5348/100130Z10SM2024CS
How to cite this article
Minzer S, Tenorio B, Descalzi B, Verdugo J, Olguin T. Superior mesenteric artery syndrome in oncology: Report of two cases and review of the literature. J Case Rep Images Oncology 2024;10(1):17–23.ABSTRACT
A rare cause of abdominal pain is the superior mesenteric artery syndrome (SMAS), characterized by an extrinsic compression of the third portion of the duodenum by the superior mesenteric artery. It occurs in the context of rapid weight loss, because of the decrease of intra-abdominal fat causing a reduction in the exit angle of this important vascular structure. Cancer patients frequently present with weight loss, often severe, making them a population at risk of presenting this syndrome. Because symptoms are vague and could be secondary to oncologic treatments, the diagnosis of SMAS is often overlooked. We present two cases of oncology patients evaluated in the National Cancer Institute in Chile who presented with symptoms suggestive of SMAS, weight loss greater than 5 kg in a short period of time associated with abdominal pain and vomiting. Both cases were confirmed by images [computed tomography (CT) scan] and treated with nutritional support only. We present both cases along with a brief review of the literature on this rare syndrome, which is usually a diagnostic challenge.
Introduction
Abdominal pain is a common symptom in cancer patients which motivates many medical consultations. A rare cause of this symptom is the superior mesenteric artery syndrome (SMAS), characterized by an extrinsic compression of the third portion of the duodenum by the superior mesenteric artery (SMA) [1],[2],[3]. The incidence described in the literature is variable, between 0.3% and 0.5% of the general population [1],[3],[4]. However, a recent retrospective study reports a higher incidence, up to 4.9% of patients under 25 years of age who presented with abdominal pain [2]. These differences in the reported incidence could be in the context of low clinical suspicion, which can delay or prevent a timely diagnosis.
Most cases of SMAS are acquired, mainly in the context of rapid weight loss. This causes a decrease in the perivascular mesenteric fat, with the consequent reduction of the exit angle of the SMA in the aorta, causing clamping of the duodenum at the level of its third portion, which is located between both structures [2],[3]. Suggestive symptoms are postprandial epigastric pain, heartburn, and early satiety when the obstruction is mild, but symptoms can progress with recurrent vomiting and greater weight loss [3]. The diagnosis is confirmed with images, demonstrating a decrease in the exit angle of the SMA (less than 22°) and a shortening of the aorto-mesenteric distance (less than 8 mm), associated with the presence of proximal duodenum dilation [1],[2],[3],[5],[6]. Management is usually medical, based on intensive nutritional support to recover visceral fat, but it can require a more aggressive treatment, including surgery in a small group of patients.
Cancer patients frequently present rapid weight loss, abdominal pain, nausea, and vomiting. Many of them may present with SMAS, however, to our knowledge, there is no report of prevalence in this population. In this article, we present two cases of oncology patients evaluated in the National Cancer Institute in Chile who presented with symptoms suggestive of SMAS and were confirmed by images, along with a brief review of the literature on this rare syndrome, which is usually a diagnostic challenge.
Case Report
Case 1
Female patient, 58 years of age, who had been treated for papillary thyroid cancer ten years earlier, presented with a right supraclavicular mass. Histological studies described a pleomorphic high-grade sarcoma. Surgical resection was performed, plus tracheostomy and gastrostomy. Blended feeding was administered through the gastrostomy. During the next four months a 15% weight loss was documented (from 45 to 38 kg), reaching a body mass index of 17.8 kg/m2. Imaging control with positron emission tomography-computed tomography (PET-CT) revealed a large local tumor recurrence, without metastasis, so treatment with doxorubicin and pazopanib was initiated. Continuous enteral nutrition with a hypercaloric formula (1.5 kcal/mL) was decided, considering preventive measures for refeeding syndrome, along with small volumes of oral liquids. Despite maintaining infusions < 50 mL/h, the patient presented recurrent abdominal pain and bloating, forcing to lower enteral infusions to 20–30 mL/h.
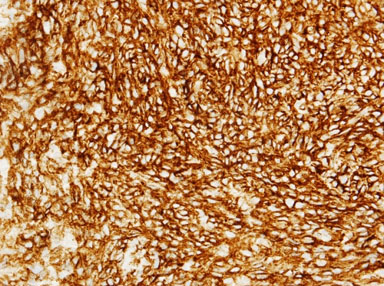
The patient presented intense epigastric pain, vomiting, and constipation, requiring hospitalization. Symptoms subsided when lowering enteral nutrition infusions up to 20 cc/h, and exacerbated when enteral nutrition volume was increased. The physical exam showed a normal abdomen, no distension, soft, with slight sensitivity at the epigastrium and no signs of peritoneal irritation. By this time, the patient’s weight was 36 kg, reaching a body mass index (BMI) of 16.8 kg/m2. An upper digestive endoscopy showed an esophageal stricture with actinic appearance, requiring endoscopic dilation. However, since stenosis does not explain the feeding intolerance, a CT scan was performed. It reported a significant decrease in intra-abdominal fat, especially in the retroperitoneal fat panniculus, associated with a change in caliber and dilation of the second and third portion of the duodenum (Figure 1 and Figure 2), possibly due to partial compression of the third portion between the aorta and the SMA. No other signs of intestinal obstruction were observed. Superior mesenteric artery syndrome was suspected so the images were reviewed with the radiologist, finding an aorto-mesenteric angle of 17° (Figure 3) and an aorto-mesenteric distance of 7.3 mm (Figure 4).
Endoscopic treatment was decided. A jejunal tube was inserted endoscopically through the gastrostomy, 55 cm distal to the pylorus. Enteral nutrition (hypercaloric 1.5 kcal/mL formula) was restarted at 20 cc/h and progressed up to 40 cc/h, with no digestive symptoms. During the next four weeks, the patient gained 3 kg, and was discharged with good tolerance to enteral nutrition, no digestive symptoms and weighing 39 kg.
Case 2
Female patient, 42 years of age. She presented a history of cervical cancer treated with radiotherapy, brachytherapy, and chemotherapy; the latter suspended after the second cycle due to cerebral thrombosis. During an annual control with PET-CT, disease progression was identified with the presence of lung metastases. Palliative chemotherapy was indicated, which was poorly tolerated, presenting intense abdominal pain that affected oral intake, causing a weight loss of 11 kg in four months. Oncologic treatment was suspended after the fourth cycle. Angio-CT of the abdomen and pelvis was performed, which described extensive ileitis with an area of segmental ischemia, not occlusive nor perforated. The study was complemented with an abdominal magnetic resonance image (MRI), which showed an inflammatory process at the level of the ileum suggestive of actinic origin, with a certain degree of dilation, wall thickening and edema of small intestine loops, especially in the pelvic cavity, without evidence of occlusion points. The patient developed intense postprandial abdominal pain, abdominal distension, and abundant explosive vomiting, with no response to pharmacologic treatment. Due to weight loss and poor response to medication, the patient was hospitalized. The physical examination revealed dry, pale mucous membranes, limpness, a distended yet depressible abdomen, diffuse pain on palpation, and no signs of peritoneal irritation. Upon admission, the patient weighed 46.7 kg, with a BMI of 17.2 kg/m2.
A free-fall nasogastric tube was installed to improve symptoms. A colonoscopy describes mild nonspecific distal ileitis, biopsies reported moderate active chronic ileitis, with subtotal villous atrophy. Computed tomography angiography showed no evidence of intestinal obstruction or mesenteric ischemia. Given the suspicion of SMAS, the images are reviewed in a targeted manner with a radiologist, identifying a decrease in the aorto-mesenteric angle of 14° (Figure 5) and a decreased aorto-mesenteric distance of 6.9 mm (Figure 6). During her hospitalization, the patient received mixed nutrition, oral and parenteral. A liquid, fractionated diet was started and postural changes were suggested during oral feeding to promote the passage of intestinal contents through the duodenum. Oral tolerance improved, but isolated episodes of vomiting persisted. Installation of a nasojejunal tube was suggested to maintain nutritional support at home, but the patient rejected this measure due to the progression of her underlying disease and the desire to remain without invasive measures at home. She was discharged after four weeks of hospitalization, with a 2 kg weight gain and better oral tolerance.





Discussion
Superior mesenteric artery syndrome is an infrequent entity, not broadly known. It was first described in 1861 by Carl Freiher von Rokitansy in autopsies and, later, Wilkie published a series of 75 cases in 1927 [6]. Because the symptoms caused are common with other pathologies, it is important to have a high index of suspicion to make the diagnosis.
Duodenal obstruction in SMAS is caused by the loss of retroperitoneal fat located between the aorta and the beginning of the SMA. This generates a decrease in its exit angle (normally between 38° and 56°) from the aorta, causing extrinsic compression of the duodenum, which passes between both vessels, and consequently obstruction to the passage of intestinal contents [6]. This obstruction can be partial or total and it can be affected by the patient’s position, improving in the left lateral decubitus or prone position as the aorto-mesenteric distance increases [5].
The diagnosis is radiological. A simple abdominal X-ray may show gastroduodenal distention that allows for suspicion, but it must be confirmed with a CT scan with intravenous contrast, which evaluates the vascular and gastroduodenal anatomy, making it the gold standard imaging technique [6]. The diagnosis is made with a reduced aorto-mesenteric angle (6–22°) or aorto-mesenteric distance (2–8 mm), in a sagittal and axial section of the CT scan [6]. According to the criteria from the study by Waheed et al., the diagnosis of SMAS is “suggestive” with a decreased aorto-mesenteric angle and distance associated with proximal dilation of the duodenum; “probable” when the angle and distance is decreased, without proximal duodenal dilation; and “possible” when there is a reduction in angle or distance [2]. Although CT with intravenous contrast in the venous phase is sufficient to make the diagnosis, the use of AngioCT provides the benefit of thinner slices (1 mm) and multiplane 3D reconstructions, which allows better visualization of the aorto-mesenteric angle and distance [6]. Moreover, the use of CT and AngioCT also allows to rule out other causes of abdominal pain that may explain the symptoms.
The treatment consists on the thickening of the retroperitoneal fat mass that allows the release of the duodenum. This entails dietary measures such as fractioning meals, changes in consistency, and postural management, to allow the passage of intestinal contents distally. More advanced measures are the use of enteral nutrition through nasojejunal tube, jejunostomy, or supplemental parenteral nutrition [7]. It is not clear how much weight must be gained to recover retroperitoneal fat mass, so symptoms must be monitored until they subside.
The SMAS has been more frequently described in young patients with a history of weight loss, in the context of spinal surgeries, anorexia nervosa, or even bariatric surgery. Although nutritional compromise is common in oncology patients, case reports of patients with SMAS are scarce [4]. We conducted a literature search in PubMed and Google Scholar, using the terms “superior mesenteric artery syndrome,” “Wilkie’s syndrome,” “oncology,” “cancer,” and “weight loss.” To our knowledge, only 16 cases of oncology patients with SMAS have been reported to this date in the literature, and are listed in Table 1.
Since abdominal pain is a frequent symptom and imaging control is a common practice, we should expect a higher rate of diagnosis. It is possible that this clinical entity is under-diagnosed because it requires a high clinical suspicion to guide the radiologist in the search for the diagnostic criteria. The lack of an accurate diagnosis, along with progressive worsening of symptoms, can negatively affect the patient’s quality of life and impair their oncologic treatment.
In both cases presented above, the diagnosis was done after several months of continuous symptoms. This causes higher weight loss, because of the constant gastrointestinal symptoms discussed, worsening the initial setting. The treatment approaches were different, but resulted in similar effects. In case 1, enteral nutrition was provided, reaching a weight gain of 3 kg in four weeks. In case 2, nutritional support was done through parenteral nutrition, along with oral feeding, reaching a weight gain of 2 kg in four weeks. Symptoms decreased in both cases, improving quality of life.
Treatment options discussed in the literature are varied, ranging from nutritional support (oral, enteral, or parenteral) to surgery. In the cases reviewed in the literature, most patients received enteral nutrition, four required a mixed approach, only five received parenteral nutrition and five patients needed surgery. The management is not standardized, nonetheless, nutritional support seems the safest option in oncology patients, often fragile and undernourished.

Conclusion
Superior mesenteric artery syndrome should be considered as a possible differential diagnosis in cancer patients who present abdominal pain and postprandial vomiting, associated with weight loss. Imaging studies, which are often frequent during cancer treatment, allow us to evaluate vascular structures around the duodenum and help rule out other common causes of abdominal pain. It is important to know this syndrome to have a high index of suspicion and thus be able to provide adequate and early management to a group of patients who need to maintain their nutritional status for their oncological treatment.
REFERENCES
1.
Ren PLJ, Gupta A. Adolescent with superior mesenteric artery syndrome. J Radiol Case Rep 2020;14(3):14–23. [CrossRef]
[Pubmed]

2.
Waheed KB, Shah WJ, Jamal A, et al. Superior mesenteric artery syndrome: An often overlooked cause of abdominal pain! Saudi Med J 2021;42(10):1145–8. [CrossRef]
[Pubmed]

3.
Ciortescu I, Nemteanu R, Hincu C, Gheorghe L, Plesa A. An underrated diagnosis of superior mesenteric artery syndrome: A case report. Diagnostics (Basel) 2022;12(9):2159. [CrossRef]
[Pubmed]

4.
Corsi NJ, Abu-Heija AA, Ravi AK, Corsi MP, Ehrinpreis MN. Wilkie’s syndrome following chemotherapy: A case report and a review of literature. Case Rep Gastrointest Med 2022;2022:7783074. [CrossRef]
[Pubmed]

5.
Merrett ND, Wilson RB, Cosman P, Biankin AV. Superior mesenteric artery syndrome: Diagnosis and treatment strategies. J Gastrointest Surg 2009;13(2):287–92. [CrossRef]
[Pubmed]

6.
Warncke ES, Gursahaney DL, Mascolo M, Dee E. Superior mesenteric artery syndrome: A radiographic review. Abdom Radiol (NY) 2019;44(9):3188–4. [CrossRef]
[Pubmed]

7.
Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig Surg 2007;24(3):149–56. [CrossRef]
[Pubmed]

8.
Lippl F, Hannig C, Weiss W, Allescher HD, Classen M, Kurjak M. Superior mesenteric artery syndrome: Diagnosis and treatment from the gastroenterologist’s view. J Gastroenterol 2002;37(8):640–3. [CrossRef]
[Pubmed]

9.
Bhattacharya D, Kamel M, McAuley D. Superior mesenteric artery syndrome (Wilkie’s syndrome) complicating recovery from posterior fossa surgery in a child—A rare phenomenon. Childs Nerv Syst 2008;24(3):365–7. [CrossRef]
[Pubmed]

10.
Bang CS, Lee SI, Park GW, et al. A case of superior mesenteric artery syndrome due to peritoneal seeding in a colon cancer patient. The Korean Journal of Medicine 2009;76(3):380–4.

11.
Ushiki A, Koizumi T, Yamamoto H, Hanaoka M, Kubo K, Matsushita M. Superior mesenteric artery syndrome following initiation of cisplatin-containing chemotherapy: A case report. J Med Case Rep 2012;6:14. [CrossRef]
[Pubmed]

12.
Girotra M, Shah HR, Rego RF. An intriguing cause of intractable nausea and vomiting. Saudi J Gastroenterol 2013;19(4):190–1. [CrossRef]
[Pubmed]

13.
Chowdhary M, Pansuria HP, Farooqi B, Goyal H. Superior mesenteric artery syndrome: A unique complication following carboplatin-based chemotherapy. Int Med Case Rep J 2015;8:55–8. [CrossRef]
[Pubmed]

14.
Lei Q, Wang X, Wu C, Bi J, Zhang LI. Superior mesenteric artery syndrome caused by surgery and radiation therapy for a brain tumor: A case report. Exp Ther Med 2015;10(4):1578–80. [CrossRef]
[Pubmed]

15.
Kitade H, Matsuura T, Yanagida H, et al. Superior mesenteric artery syndrome after ileal pouch-anal anastomosis for colon cancer associated with ulcerative colitis: Report of a case. Surg Case Rep 2015;1(1):27. [CrossRef]
[Pubmed]

16.
Irie Y, et al. Superior mesenteric artery syndrome after esophagectomy for esophageal cancer. Diseases of the Esophagus 2016;29:PS01.077.

17.
Garg S, Derzie A. A rare case of gastric mantle cell lymphoma causing superior mesenteric artery syndrome in an adult. Int J Angiol 2016;25(5):e73–6 [CrossRef]
[Pubmed]

18.
Takehara K, Sakamoto K, Takahashi R, et al. Superior mesenteric artery syndrome improved by enteral nutritional therapy according to the controlling nutritional status score. Case Rep Gastroenterol 2017;11(3):729–35. [CrossRef]
[Pubmed]

19.
Haider A, Sharma M, Siddiqa A. Superior mesenteric artery syndrome: A forgotten cause of duodenal obstruction. Cureus 2020;12(9):e10710. [CrossRef]
[Pubmed]

20.
Wong LH, Sutton TL, Spurrier RG, Zigman AF, Mayo SC. Post-operative superior mesenteric artery syndrome following retroperitoneal sarcoma resection. Clin Pract 2020;11(1):2–7. [CrossRef]
[Pubmed]

21.
Kim J, Yang S, Im YC, Park I. Superior mesenteric artery syndrome treated successfully by endoscopy-assisted jejunal feeding tube placement. BMJ Case Rep 2021;14(11):e245104. [CrossRef]
[Pubmed]

22.
Zhou Y, Yang ZL, Wang Z. Superior mesenteric artery syndrome following esophageal cancer surgery: A report of two cases and a literature review. Med Int (Lond) 2022;2(2):10. [CrossRef]
[Pubmed]

23.
Miyadera K, Nakamichi S, Miyashita R, et al. Two cases of superior mesenteric artery syndrome during chemotherapy in patients with lung cancer. Int Cancer Conf J 2022;11(2):124–8. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Simona Minzer - Substantial contributions to conception and design, Analysis of data, Interpretation of data, Drafting the article, Final approval of the version to be published
Beatriz Tenorio - Acquisition of data, Analysis of data, Revising it critically for important intellectual content, Final approval of the version to be published
Bárbara Descalzi - Acquisition of data, Analysis of data, Drafting the article, Revising it critically for important intellectual content, Final approval of the version to be published
Jaime Verdugo - Acquisition of data, Analysis of data, Interpretation of data, Drafting the article, Final approval of the version to be published
Thiare Olguin - Substantial contributions to conception and design, Acquisition of data, Analysis of data, Interpretation of data, Revising it critically for important intellectual content, Final approval of the version to be published
Data Availability StatementThe corresponding author is the guarantor of submission.
Consent For PublicationWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Competing InterestsAuthors declare no conflict of interest.
Copyright© 2024 Simona Minzer et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.